|
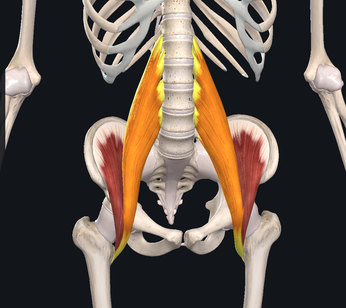
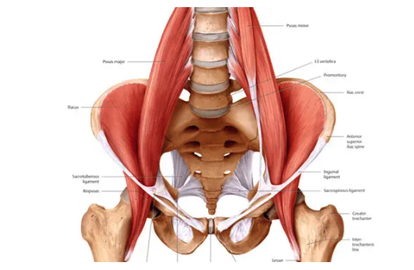
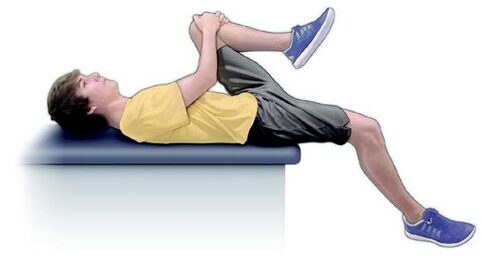
We've spent the last few Muscle Mondays focusing on the upper body, particularly about posture and how it affects our muscles and joints. Let's take a moment and look at one of the integral team members of our "core" and a common culprit for low back-related issues. Allow me to introduce to you, the Psoas Major (silent "P"). While there are many unique features about this muscle, perhaps the most significant is the number of joints that it crosses. This muscle originates at the transverse processes of T12-L4, crossing 5 spinal segments before going distally and inserting into the lesser trochanter of the femur. Because it crosses so many joints, it is responsible for 3 main movements including: Lumbar flexion, ipsilateral side-bend and hip flexion. Because of its attachment on the inside of the thigh, it also will slightly externally rotate the femur as well. Trunk/Lumbar flexion Trunk/Lumbar Sidebend Hip Flexion The primary job of the Psoas is to flex the hip. It joins together with the iliacus muscle to form the iliopsoas tendon. One of the main issues that people commonly face, particularly those who have a more sedentary lifestyle or job that requires several hours of sitting, is that the muscle will gradually adapt and shorten over time. Why this is an issue, is that this can result on increased stress on the lower back when you try and stand up tall/straight due to the tightness of the muscle which naturally would pull you into more trunk and hip flexion. In order to compensate, you would extend (or arch) your back more to allow you to get into the full upright position. Other common issues related to the psoas major are hip flexor tendinitis and/or "snapping hip syndrome" (the two are NOT synonymous). Hip flexor tendinitis describes an acute inflammation of the iliopsoas tendon and commonly painful with active contraction of the hip flexors. On the other hand, snapping hip syndrome is a condition in which a person may experience or hear a popping/snapping sensation in the front of their hip when they flex their hip, but may or may not be painful when the sensation occurs. Snapping hip syndrome typically indicates that there is friction on the tendon (which causes the "snap"). It could potentially lead to tendinitis and scar tissue formation of the iliopsoas tendon. Both of these conditions are commonly found in dancers, bikers, soccer players and runners. One quick and simple way to check to see if you have tight hip flexors is to perform a Thomas Test. While this is most commonly performed by a healthcare professional in the clinic, it is simple to do and can offer helpful insight to help you fine tune your body. To perform, you lay down on a bed while hugging one knee towards your chest. The other leg (the one you are testing) would drop down towards to floor. If you feel your back start to arch up, or if your femur (thigh) does not reach parallel to the floor, it would suggest that you have tightness/stiffness of your hip flexors. Do not, however, perform this if you are unsteady (in other words, don't fall off the bed), or if you already have pain in the area. Please make sure to seek advice from a medical professional for more detailed assessment. One very simple and easy place to start would be to start a simple stretching and strengthening regimen. Follow along in the video below to learn one of my all-time favorite stretches that I personally do on a daily basis. Of course, this is all about balance. Not only is stretching largely advisable to help maintain good habits, but it is also important to strengthen the appropriate muscles as well. In this particular case, it is important to focus on the glutes (Max, Med). Make sure that if you sit for work or school, that you get up and stretch a couple of minutes or walk around every hour. As always, check in with your friendly neighborhood physical therapist for specific guidance and tips to help you keep your body in prime working condition.
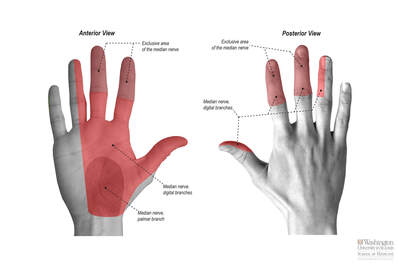
Until next time, Opus Fam! Carpal Tunnel Syndrome (CTS) is one of the most commonly known wrist/hand injuries. This ailment is often found in the sedentary desk job population, grocery checkout clerks, and other occupations associated with high quantities of repetitious movements -- including..... MUSICIANS. As seen in the first image below, there are 3 major nerves that provide sensation to the hand. They include the Median Nerve, Ulnar Nerve, and the Radial Nerve. What is important to note, is that these nerves originate from the brain and are comprised of several cervical nerve roots in the neck before joining together to form the awesome super-highway nerves listed above. CTS specifically describes the impingement of the Median Nerve at the level of the wrist. With CTS, the distribution of symptoms follows a specific pattern. Most commonly, patients will complain of symptoms on the PALMAR aspect of their hand including the thumb, index, middle fingers as well as 1/2 of the ring finger (side closest to the middle finger). It is very important to know this when trying to figure out which nerves may be affected, because the Ulnar and Radial Nerves will affect OTHER portions of your hand (to be discussed at a later date). Common symptoms include:
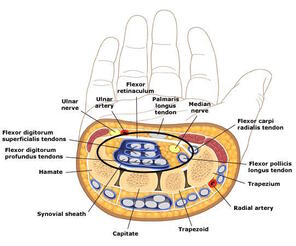
CTS occurs when there is too much pressure within the carpal tunnel, a VERY small space where 9 tendons and the Median nerve pass through in order to go into the hand. As you can see, there is not a whole lot of space for error. So - when we subject our bodies to high stress/repetitive activities, inflammation and swelling can occur which can cause more pressure on the nerve. How would you like it if someone tried to squeeze their body into an already jam-packed elevator? You would be irritated. That's how your nerve is probably feeling. You: "Ok, Janice. I've done my research, and I think I have CTS. What do I do?"
First of all, it is not entirely advisable that you self-diagnose your problems. What IS advisable, is that you do your research as you have, AND consult a KNOWLEDGEABLE healthcare professional, such as a physical therapist or orthopedist. Conservatively, there are a few things you can try to decrease your symptoms:
That's all for now. Be happy and healthy! |
AuthorDr. Janice Ying is a Los Angeles-based Physical Therapist. She is board-certified Orthopedic Physical Therapy Specialist and is regarded as a leading expert in the field of Performing Arts Medicine and the development of cutting edge injury prevention and rehabilitation programs for musicians. DisclaimerThe information on this website is intended for educational purposes and should NOT be construed as medical advice. If you have or think you have a health-related issue which needs to be addressed, please seek the help from your local licensed medical professional.
Archives
October 2020
Categories
All
|
We would love to see you soon!
|
© Opus Physical Therapy and Performance - 2021 - All Rights Reserved

 RSS Feed
RSS Feed